With age, many of us develop a cluster of symptoms known as Metabolic Syndrome. In general terms, the components of Metabolic Syndrome are central obesity (belly fat), poor glucose metabolism, high blood pressure, and unhealthy blood lipids.
There are several proposals for the exact definition. The National Cholesterol Education Program 2005 defines Metabolic Syndrome as any 3 of the following conditions:
Glucose > 100 mg/dL, or drug treatment for diabetes.
Triglycerides > 150 mg/dL, or drug treatment
Blood pressure > 130/85 mmHg or drug treatment
Waist > 35 inches for women (40 inches for men).
The World Health Organization definition uses a waist/hip ratio > 0.85 for women (0.9 for men) as the criterion for central obesity, while the International Diabetes Federation uses a tighter definition of waist > 31 inches for women, 37 inches for men.
The significance of Metabolic Syndrome is controversial. All the criteria are related to unhealthy lifestyles, age, risk for developing diabetes, and risk for cardiovascular disease. Is Metabolic Syndrome a disease on its own? These symptoms occur together often enough to attract considerable interest in the medical literature. What is the connection? Does obesity cause the other problems? And why does it matter how the fat is distributed, as in the waist/hip ratio? (For more on this, see https://www.empowher.com/news/herarticle/2009/08/26/woman’s-heart-how-round-too-round).
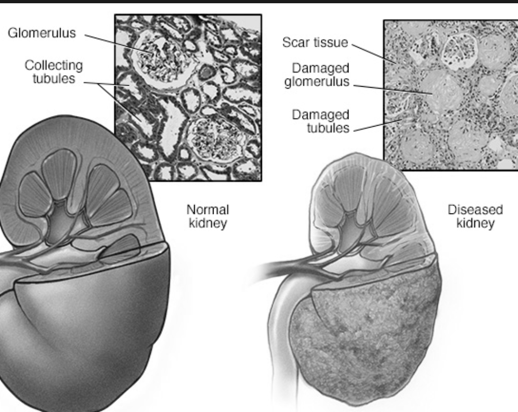
An article in the Journal of Nephrology offers another possibility. A link between Metabolic Syndrome and Chronic Kidney Disease (CKD) is emerging in cardiorenal research. The early stages of kidney dysfunction could be the root problem. If the kidneys are not functioning at 100%, then a number of chemicals appear in elevated concentration in the bloodstream. These are called uremic retention solutes, and include:
1. oxidative stress products
2. pro-coagulant factors
3. interleukin-6
4. phosphate and calcium-phosphate product
5. asymmetric dimethylarginine
6. parathyroid hormone
7. neuropeptide Y
8. homocysteine
9. phenylacetic acid
10. indoxyl suophate
11. guanidine, methylguanidine, guanidinosuccinic acid, and guanidinoacetic acid
12. p-cresol
Abnormally high concentrations of anything that is supposed to be eliminated by the kidneys is suspect in causing cardiovascular disease. On the other hand, the cause and effect relationship between Metabolic Syndrome and chronic kidney disease is not clear. Either one could cause the other, or some other factor may cause both. In any case, that middle age spread around the middle is a reminder to keep up with our check-ups.
References:
Natali A et al, “Metabolic syndrome: at the crossroads of cardiorenal risk”, J Nephrol 2009; 22:29-38.
Vanholder R et al, “Chronic kidney disease as cause of cardiovascular morbidity and mortality”, Nephrology Dialysis Transplantation 2005; 20:1048-1056.




Add a CommentComments
There are no comments yet. Be the first one and get the conversation started!