Back in 1985, peritoneal dialysis sounded like the ultimate answer for kidney failure. I heard the seminar by Professor Popovich, one of the creators of the technique, at The University of Texas. Kidney patients no longer had to be hooked up to a machine in a medical facility for hours on end, every day of their lives.
Peritoneal dialysis offered them the freedom to go home and live a normal life. One of the slides in that seminar was a picture of a smiling man holding a beer mug. “You can even drink beer on this treatment,” Popovich told us.
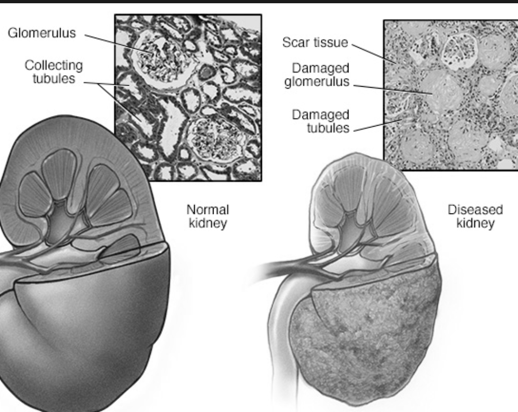
The reality has been less revolutionary. Peritoneal dialysis makes use of the fact that the peritoneal membrane is actually a closed sack in our abdomens. It's possible to pump a solution of glucose into this sack. Water and small molecules diffuse from the blood vessels in the membrane into the glucose solution. The patient can change the solution a few times per day. This mimics what the kidneys do in healthy people.
Unfortunately, the peritoneal membrane is much less efficient than the kidneys. Too much potassium and too little phosphate are removed by this treatment. Proteins and amino acids are removed at a rate high enough to produce malnutrition. Glucose from the dialysate solution diffuses into the blood stream and contributes to development of abnormal blood lipids. These problems can be corrected to some extent by a special diet. The synthetic membranes used in traditional hemodialysis have similar issues.
Today, kidney transplant patients survive longer and have a better quality of life than patients on either hemodialysis or peritoneal dialysis. Even with the risks of organ rejection and immunosuppressive drugs, a human kidney can do a much better job than either dialysis method. But there are far more patients who need kidneys than there are donors. So doctors and patients would like to know which of the available dialysis treatments offers the best results.
Ideally, medical researchers would like to do a randomized clinical trial of peritoneal dialysis and hemodialysis. This has not been done because there are not enough patients willing to be randomized. According to a group of Canadian researchers, patients who are informed about their treatment options generally develop a strong preference for one or the other. So observational studies are the main source of information about the relative risks and benefits of the two techniques. These risks and benefits change with time spent in treatment. The authors of Reference 2 describe many complications in the analysis of available data. They point out that after more than 20 years of peritoneal dialysis treatment, we still need studies to provide the answers that patients and doctors need to make an informed choice for or against this technique.
References:
Wu G et al, “Continuous ambulatory peritoneal dialysis: no longer experimental”, Can Med Assoc J 1984 March 15; 130: 699-706.
Quinn RR et at, “Comparative studies of dialysis therapies should reflect real world decision-making”, Journal of Nephology 2008; 21:139-45.
Linda Fugate is a scientist and writer in Austin, Texas. She has a Ph.D. in Physics and an M.S. in Macromolecular Science and Engineering. Her background includes academic and industrial research in materials science. She currently writes song lyrics and health articles.



Add a CommentComments
There are no comments yet. Be the first one and get the conversation started!